Breasts come in different shapes, sizes and densities.
In some cases, dense breast tissue can be associated with an increased risk of breast cancer.
A 2017 U.S. study revealed that four in 10 cases ofbreast cancerin younger women can be blamed on high breast density. The results show that breast density is a much more important breastcancer risk factorto be aware of than a person’s family history. But having dense breasts is not an abnormal condition. In the United States, 43% of women over the age of 40 have dense breast tissue. It’s basically a physical attribute of the body and there’s little anyone can do to actively change or improve the density of their breast.
Annual screenings are important
Allison Gleason, RT (R) (M), an OSF HealthCare supervisor of mammography and ultrasound, said it’s important to remember that the density of a woman’s breasts can change over time. That’s why it’s important to get annual mammogramscreeningsto stay up-to-date on the condition of your breasts. Remember to continue to getting routine screening mammograms even when additional exams are suggested for you.
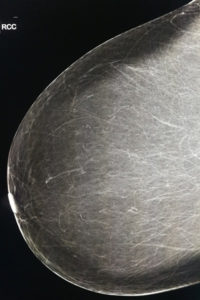
Breast tissue consists of fatty and fibroglandular tissue. Dense breast tissue is defined as having a higher percentage of fibroglandular tissue within your breasts. If more than 50% of your breasts is made of fibroglandular tissue, then your breasts are classified as “dense.”
The more fibrous and glandular tissue absorbs more radiation during mammography, reducing the accuracy of the test and making it more difficult to properly diagnose breast cancer. Dense breast tissue shows up white on a mammogram, as do tumors, which makes it more difficult to identify the difference.
According to the American Congress of Obstetricians and Gynecologists, amammogramwill identify 88% of cancers in a breast that is almost entirely fat, or low in density. That’s compared to 62% in high-density breasts.
State laws
“2019年1月1日,伊利诺伊州开始要求对乳房x光检查患者通报他们有致密的乳房组织。密歇根州自2015年起就有了这项法律,”艾莉森说。被告知乳腺组织致密是一种常见的正常现象。”
Dense breast tissue may obscure or hide breast cancers on a mammogram –– potentially delaying diagnosis in these women. Both dense breast tissue and cancer appear white on a mammogram, creating a dangerous camouflage effect and a dilemma for radiologists whose goal is to find breast cancer as early as possible. ABUS will allow us to better meet the health needs of women as they receive their annual screenings.
Had your annual mammogram?
“If you happen to be a patient that has been identified as having dense breast tissue, it is important to understand your options to ensure the best possible imaging studies are performed for confidence in imaging results.”
Imaging techniques
Two of the best imaging techniques for screening dense breast tissue include having 3D (tomosynthesis) yearly with your annual screening mammogram andABUS (Automated Breast Ultrasound)once identified as having dense breasts. 3D mammography has been shown to greatly reduce detection challenges associated with overlapping structures in the breast. The low-dose 3D mammogram exam takes just 3.7 seconds per view resulting in greater patient comfort and a reduced chance of patient motion.
Once having a screening mammogram, the radiologist may recommend an ABUS,
which is being used to detect breast cancer in women with dense breast tissue. ABUS is demonstrating a 35.7% improvement in detecting breast cancer in women with dense breast tissue that have not had a prior issue. The exam allows radiologists to look through hundreds of image slices to determine and locate breast cancer that may not have been detected by a regular mammogram.
With an order from a primary care provider, ABUS can be scheduled to be completed during the same setting as an annual mammogram.
What to do
If you receive a report indicating you have dense breast tissue,speak with your doctorabout your breast tissue density and family history of breast cancer to determine the best imaging options. Additionally, you should check with your insurance provider for coverage on 3D (tomosynthesis) and ABUS.
